Oral mechanism exam, oral motor exam, oral-facial exam, oral peripheral exam, oral-mech exam… whatever you call it, it’s one of the most important, but frequently neglected, components of an initial assessment for any child with a suspected speech sound disorder. In fact, as outlined in ASHA’s Practice Portal regarding Speech Sound Disorders, an oral mechanism examination is a key component of a comprehensive speech evaluation. Completing a thorough Oral Mechanism Exam (OME) helps us as SLPs determine if the structure and/or function of the speech mechanism is even adequate for speech production.
Now, I know we’ve all had those kids that pop up on our caseloads that look like clear-cut, straightforward “just artic” cases. A quick Goldman-Fristoe and language sample shows that the only issues seem to be one or two speech sound errors. Should be a pretty quick fix, right? Then, low and behold, years go by and that child is still in speech therapy working on those same sounds. Or perhaps you’re treating a child who is so highly unintelligible that you suspect Childhood Apraxia of Speech, but don’t really have a clear picture of his or her speech/oral motor abilities, so making a definitive diagnosis is proving to be tricky. What about that child who may only present with a couple of speech sound errors, but those errors tend to be hypo- or hypernasality and they just don’t seem to be stimulable for the target sounds at all? What’s a clinician to do?
I frequently receive queries from other SLPs asking for tricks and tips for treating just such cases. But, before I even address appropriate therapeutic intervention strategies, my first question is almost always, “what did the oral-mech exam show you?”. If we haven’t found or ruled out underlying structural or functional issues, then we may be using the wrong approach in therapy.
So let’s talk about what a good oral-mech exam (OME) can help you determine:
Structure
There may be actual physical abnormalities that impact speech production, such as any significant asymmetries, atypical dentition, the presence of dental appliances, abnormalities of the palate, like clefting or a bifid uvula, enlarged tonsils, or other unusual growths, just to name a few. If the actual structure of the oral mechanism is compromised then a referral to a specialist (ENT, craniofacial team, neurologist, dentist, etc.) may be appropriate and therapy may need to focus more on compensatory strategies.
Function
An OME should also systematically assess how each articulator performs motor tasks, addressing strength, range of motion, speed of movement, whether extraneous movements are noted, and if any groping is observed during volitional motor tasks. These observations are key in helping us differentially diagnose the dysarthrias and oral apraxia, as well as determining if further assessment is warranted, such as myofunctional or motor speech assessments.
I have also come to realize that a good OME can not only help us be more confident in making differential diagnoses and determining what types of therapeutic interventions will be most appropriate, but it can also give us important clues about what types of supports will benefit a particular child. For example, if you have a child who is extremely averse to touch, has a hyperactive gag reflex, or just doesn’t want you anywhere near their mouth, then tactile prompts may not be a good option. Relying on visual and verbal prompts may be your best bet, at least initially. In addition, if a child shows difficulty moving the tongue independently from the jaw, for example, then focusing on jaw/tongue dissociation should also be a consideration in therapy, especially if speech errors involve lingual sounds.
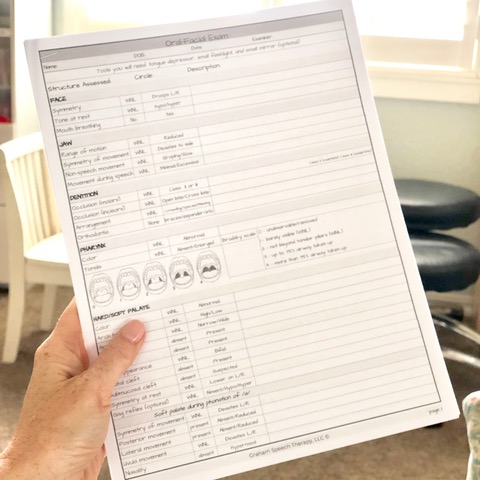
Don’t let another child with a speech sound disorder be added to your caseload without doing an OME… you never know how it may change your entire therapy approach! All you need is the Oral-Facial Exam form, a tongue depressor, a flashlight and you’re ready to go!
I hope I’ve managed to explain some of the benefits of administering a thorough OME with each child you assess for speech sound disorders. It’s why, several months ago, I went on the hunt for an exhaustive, but easy to use oral-mech exam form to use at my practice. Now that I own my own private practice that specializes in speech sound disorders, I wanted to find a checklist-style oral motor assessment form to help me be thorough, yet efficient in its administration. Since that proved to be difficult to find, I began creating an Oral-Facial Exam for my own use. But, I quickly found that not only were there other SLPs who were looking for something similar, but many didn’t feel like they had the knowledge to know how to interpret the results. So, I spent a little more time, did more research, and added detailed instructions, guidelines, and even diagrams to help any SLP identify and rule out structural/functional deficits, determine if those deficits impact speech production, and decide when to consider appropriate referrals to specialists.
Amy Graham, MS, CCC-SLP has been a speech-language pathologist for 20 years and is the owner of Graham Speech Therapy, a private practice in Colorado Springs specializing in speech sound disorders. She is listed on the Apraxia Kids Directory of SLPs with expertise in Apraxia and is PROMPT trained. She has worked in a variety of settings, from numerous public/charter schools, acute care/rehabilitation hospitals, an audiology clinic, and now private practice. Amy is committed to raising awareness about Childhood Apraxia of Speech and supporting and equipping SLPs to provide evidence-based therapy through her social media accounts on Instagram and Facebook.

If you are a parent in Austin, TX and looking for support for your child, please contact me to discuss your options.
Start Playing With Purpose
Learn how to purposefully and intentionally interact with your child during play and help them increase opportunities for speech and language development with our Playing with Purpose book!











